Telehealth Coverage and Payment (Pre-COVID-19)
Restrictions on coverage and payment of telehealth services exist today. At the federal level, coverage and reimbursement rules for telehealth under the Medicare program are defined in §1834(m) of the Social Security Act (4) (42 U.S.C. 1395m(m)(4)) which was enacted over 20 years ago and remains in effect today. The law limits payment for telehealth services to rural geographic areas, certain types of facility-based originating sites, certain types of providers, limited types of services, and audio-visual technologies. Legislative actions in 2018[13],>[14] removed the geographic and originating site restrictions to create nationwide payment for tele-stroke, end-stage-renal disease (ESRD) and substance use disorder (SUDs) treatments.
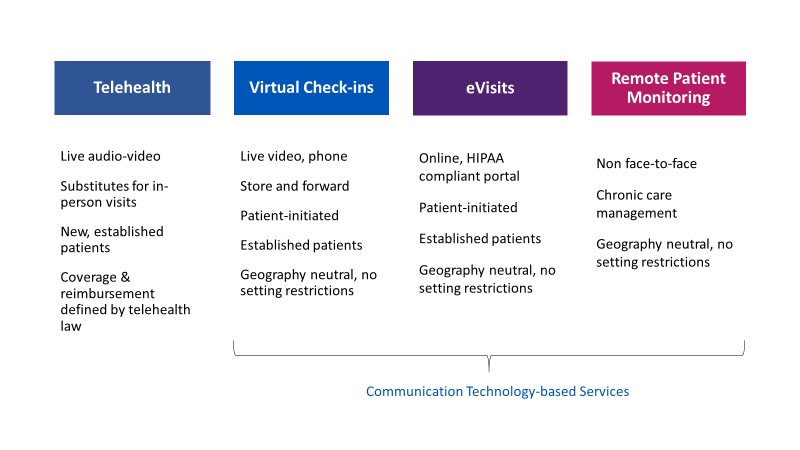
At the regulatory level for Medicare, CMS implements regulatory policy changes for telehealth and other communication technology-based services (CTBS) through the annual physician fee schedule process. A telehealth visit must substitute for an in-person visit (e.g. patient present) and be furnished via real-time, two-way audio-video technologies. For CY 2020, there are 112 billing codes on the Medicare telehealth list.[15] CMS also reimburses providers for CTBS services furnished to Medicare beneficiaries via synchronous (phone and video) and asynchronous (store and forward) brief virtual check-ins, eVisits (digital visits through an online portal), and remote patient monitoring (RPM). CMS does not consider CTBS to be “telehealth,”[16] therefore, payment for these services is not constrained or subject to the rural geographic, originating site and other requirements defined in the statute. [See CMS types of services in Figure 1]
In the shift to value-based care, CMS has targeted Medicare Advantage plans, ACOs, and bundled payments that reimburse providers based on their ability to improve quality of care in a cost-effective manner or lower costs while maintaining standards of care. Under value-based payment models, CMS offers more flexible rules for using telehealth to deliver care (e.g. no geographic restrictions, the home may serve as a qualified originating site, etc.)[17]
At the state level, states have great flexibility in shaping their own rules for telehealth coverage and reimbursement under Medicaid. Thus, policies for telehealth vary from state-to-state, with 51 different sets of rules and requirements including Washington, D.C.[18] Some states also adopt laws for how telehealth is covered and reimbursed by the private payers. These laws are often times referred to as the “telehealth private payer parity laws.” These types of laws also vary widely from state-to-state with some states addressing only “coverage” parity, which requires private payers to cover telehealth services to the same extent that the plan covers services for in-person care, while other states address both coverage and payment. Today all 50 states and DC reimburse for live, audio-video telehealth under Medicaid fee-for-service and the vast majority of states have a coverage parity law in place.[19] The Center for Connected Health Policy’s (CCHP) Fall edition of “State Telehealth Laws and Reimbursement Policies” summarizes current telehealth policies, laws, and regulations across the nation. States and private payers are also adopting value-based models under both fee-for-service and managed care.
COVID-19 Public Health Emergency (PHE) Policy Changes
When the COVID-19 pandemic arrived, policymakers took action aimed at removing many of the restrictions on telehealth to drive rapid adoption and utilization during the crisis. At the federal level, Congress quickly passed three pieces of historic legislation with major policy changes for telehealth and substantial funding for telehealth infrastructure through grants and funding awards. These legislative changes and the emergency authorities granted to the Department of Health and Human Services and at the state level set the ball in motion for a series of major policy changes that enabled broad reimbursement of telehealth in the Medicare program during the PHE. Below are key interim temporary rule changes for telehealth services during the COVID-19 PHE:
- Removes the geographic and originating site restrictions to allow providers to serve patients in all areas of the country and in all settings including at home.
- Provides reimbursement for telehealth services at the same rate as in-person visits for all diagnoses, not just services related to COVID-19 (e.g. pays both facility and non-facility rates.)
- Expands range of eligible providers who can be paid for furnishing telehealth services including FQHCS, RHCS, PTs, OTs, SLPs.
- Expands modalities that can be used to provide telehealth to include audio-only / telephone services.
- Expands eligible telehealth services that can be billed (over 120+ acute, ambulatory, and other services added to the list.)
- Enforcement discretion of HIPAA requirements allows flexibility for telehealth via popular video chat applications such as FaceTime or Skype.
- Allowances for providers to reduce or waive cost-sharing requirements for telehealth visits.
The full listing of covered Medicare telehealth services during the COVID-19 PHE and those services that are reimbursed using audio-only technologies may be found here.
Expanded coverage and payment policies for FQHCs and RHCs during the COVID-19 crisis may be found here.
CMS also expanded coverage and reimbursement policies for use of other digital health tools during the PHE including virtual check-ins, eVisits, telephone visits, and RPM. Key policy changes included:
- expansion of services to both new and established patients
- expansion of eligible providers who can bill for services
- expansion to both acute and chronic conditions for RPM
States also took rapid action that temporarily removed policy barriers to telehealth to address the COVID-19 PHE. Similar to CMS, Medicaid and the private insurers expanded coverage and reimbursement policies for telehealth including use of audio-only/telephone and allowed cost-sharing waivers of co-pays and other fees.
Coverage and reimbursement policy changes implemented by both governmental programs and private plans during the PHE will expire unless policymakers take action to make changes permanent. At the federal level, temporary policies for telehealth will end when the public health emergency period expires unless Congress takes action to pass legislation and/or CMS adopts new rules. Some states and private plans have already taken steps to adopt COVID-19 PHE changes on a permanent basis while others have reverted back to pre-COVID policies and rules.
Medicare Billing – Place of Service, Modifiers, Frequency
| Medicare | Pre-COVID-19 PHE | During COVID-19 PHE |
| Telehealth |
|
|
| Virtual Check-ins, eVisits, RPM |
|
|
State Medicaid programs and private payer policies and guidance on telehealth and other types of technology-enabled services can be found on their respective websites.
Sources
- CMS
- CMS MLN Medicare Telehealth
- CMS General Telehealth Information
- CMS Chronic Care Management
- CMS MLN Use of Modifier for Telestroke
- CMS Claims Processing Manual, Chapter 12
- CMS Interim Final Rule with Comments 1
- CMS Interim Final Rule with Comments 2
- CMS MLN CY2020 Physician Fee Schedule PHE Interim Final Rules
- CMS MLN Summary of Policies During PHE
- CMS FAQs on Medicare FFS Billing
- Listing Medicare Telehealth Codes COVID-19
- HHS Telehealth
- CMS Telehealth Video: Medicare Coverage and Payment of Virtual Services
- Center for Connected Health Policy – cchpca.org
- American Telemedicine Association – americantelemed.org
Policy Recommendations
- Providers
- Stay apprised of coverage and reimbursement policy changes and timelines and plan for a post-pandemic policy landscape when temporary changes may expire.
- Keep team informed and provide training (virtual) on policy changes, reimbursement opportunities, documentation, compliance, appropriate use of telehealth (e.g. when to use video vs audio), etc.
- Leverage all opportunities for billing telehealth and CTBS.
- Create plans/strategies that position telehealth for long-term sustainability.
- Implement telehealth infrastructure/programs to learn how to do telehealth, build team, expertise, etc., to be prepared for any future pandemic. Make telemedicine part of normal day-to-day operations.
- Policymakers
- Adopt/maintain continued broad coverage and payment policies for telehealth and other communication technology-based services to incentivize provider investment in infrastructure/drive adoption to be ready for any future pandemic, as well as to enable equity in healthcare access and connectivity and transformation to value-based care.
- Remove geographic and originating site restrictions to enable healthcare access equity and care into the home.
- Expand range of authorized providers (e.g. FQHCs, RHCs, PTs, etc) who can receive payment for telehealth and other services.
- Allow a valid practitioner-patient relationship to be established by telehealth without requiring an in-person encounter.
- Hold providers to the same standard of care as in-person care and allow providers to decide when/if a service is clinically appropriate for audio-video, audio-only, store and forward, etc.
- Align reimbursement rates to modalities (e.g. video vs audio-only.)
- Redefine “telehealth” as audio-video only to allow use of audio-only technologies when clinically appropriate.
- Remove supervision and frequency limitations attached to reimbursement of telehealth services for inpatient critical care and inpatient subsequent care (hospital and SNFs)
- Create telehealth reimbursement for home health agencies.
- Adopt/maintain coverage and payment parity policies in the short term beyond the COVID-19 PHE to maintain financial incentives to allow adoption levels to stick, build infrastructure, expand the period of time to collect data from which to base future payment policy changes.
- Create funding opportunities through grants and other mechanisms to provide support for telehealth/telecommunications infrastructure to be ready for any pandemic.
- Establish rules and guiding principles for hospitals to remain open during a pandemic.
- Align policies, standardize billing codes and modifiers among payers to reduce complexity/confusion and make it easier on providers to react to pandemics in the future.
- Provide clear, accessible guidance/resources on telehealth rules and regulations during a pandemic.
- Adopt/maintain continued broad coverage and payment policies for telehealth and other communication technology-based services to incentivize provider investment in infrastructure/drive adoption to be ready for any future pandemic, as well as to enable equity in healthcare access and connectivity and transformation to value-based care.
